Your intervention can increase cessation rates even for patients who are not ready to quit
A meta-analysis showed that a physician’s advice of 3 minutes or less:
Increased the likelihood of smoking cessation by 30%
Increased the likelihood of abstinence by 29%2
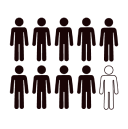
9 out of 10 patients said they welcomed counselling advice from their physician on quitting smoking.3
The 3 A’s of QC: Ask, Advise, Act
Step 1: Ask
“Have you used any tobacco products in the past week/month/3 months?”

Step 2: Advise
Offer advice in an encouraging, supporting, empathetic manner:
“Quitting on your own can be tough. We now know that counselling combined with treatment can improve your chances of success.”Advise that the best results are typically achieved with pharmacotherapy and support
Step 3: Act
Refer to counselling, internet programs and telephone quit lines
Offer examples of where patients can get support, such as a smoking cessation counsellor, a nurse at a clinic, the Canadian Cancer Society Smokers’ helpline:
“You may want to contact the Canadian Smokers’ helpline. They can help you get started. Here’s their number.”Consider nicotine replacement therapy
Let patients know help is available when they are ready to quit.
Tips to help patients trying to quit5
Manage expectations: quitting often takes several attempts
Be persistent: try not to be discouraged by a relapse; use it as a learning experience for both of you
Make repeated contacts: every visit is an opportunity to counsel your patients
Help your patients take the next step: encourage your patients to take the next step towards quitting smoking
Bolster self-efficacy and motivation: encourage your patients to believe in themselves and their ability to quit
Match your strategy to the patient’s stage of change (e.g., motivating vs. creating a plan)
Tips for being motivational
Focus on providing:
Appropriate empathy
Non-judgmental advice
Personalized feedback (reflected back to patients)
Positive reinforcement
Motivational strategies can:
Support self-efficacy
Promote autonomy
Be applied when patients are unready, unwilling, or unable to quit smoking
Tailored approaches to help your patients quit
Avant l’abandon
(Avant la date d’abandon fixée)
Post-cessation
(After fixed quit date)
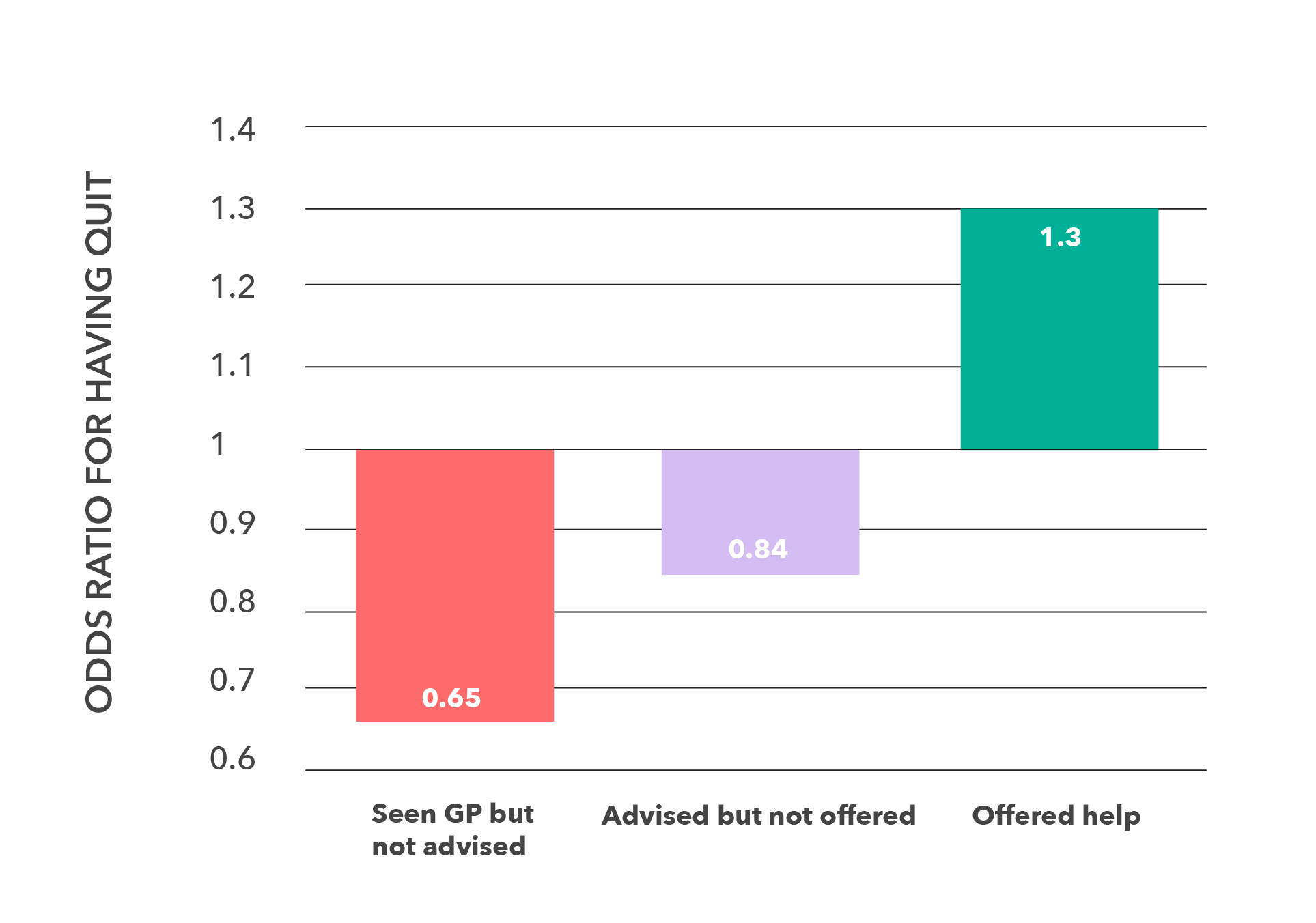
Significantly more patients quit smoking after receiving advice from their physicians4
References
1. Fiore MC, Jaén CR, Baker TB, et al. A Clinical Practice Guideline for Treating Tobacco Use and Dependence: 2008 Update. Am J Prev Med 2000;35(2):158-176.
2. Fiore MC, Jaén CR, Baker TB, et al. Clinical Practice Guideline: Treating Tobacco Use and Dependence: 2008 Update.
3. West, R. Enhancing Motivation to Stop Smoking: From Theory to Practice. Cancer Research UK. UK Centre for Tobacco Control Studies: A UKCRC Public Health Centre of Excellence. August, 2014.
4. West R. The science, economics and politics of tobacco control. University College London clinical presentation 2013. Available: http://www.uksbm.org.uk/wp-content/uploads/2014/07/robert-west.pdf.
5. MDQuit.org. Module 3: The Stages of Change. Available at: http://mdquit.org/fax-to-assist/module-3. Accessed May 11, 2015.
6. Shiffman S, Ferguson SG. Nicotine patch therapy prior to quitting smoking: a meta-analysis. Addiction 2008:103(4):557-63.
7. Reid R, et al. Managing smoking cessation. CMAJ 2016 188(17-18).
8. Cahill L, et al. Pharmacological interventions for smoking cessation: an overview and network meta-analysis. Cochrane Database Syst Rev 2013; Issue 5.